
Cervical osteochondrosis is a type of dystrophic change in the intervertebral discs in the neck.
Not only the intervertebral discs themselves are negatively affected, but also the vertebrae, soft and cartilage tissue. The main feature of the cervical spine is the fact that its vertebrae do not have the most reliable structure compared to other regions, which makes this area very fragile. The vertebrae are in close proximity to each other and to the arteries that supply the human brain.
With a displacement of the vertebrae, there is a high probability of compression of the nerve bundles and arteries, which inevitably leads to the appearance of a hernia between the vertebra and protrusion, i. e. Changes in the structure of the intervertebral disc.
What is it?
Osteochondrosis of the cervical spine (osteohondroz) is a degenerative-dystrophic lesion of the intervertebral discs, as a result of which the intervertebral discs themselves, vertebrae and joints of the cervical spine are damaged, and a decrease in the height of the intervertebral discs is observed. The disease progresses untreated and can lead to headaches, poor circulation, and even hernias. Like osteoporosis, the disease occurs due to a violation of mineral metabolism, which makes bones and joints weaken.
Why does osteochondrosis occur?
Although degenerative changes in the intervertebral discs of the cervical spine are viewed as a disease in conventional medicine, from the point of view of osteopathy they are only a manifestation of deeper disorders in the body.
Thus, the real causes of cervical osteochondrosis are:
- Muscle cramps. . . Spasmodic reactions in the back, chest and pressure muscles can lead to certain parts of the body being very tense. This disturbs the general equilibrium position of the body, which leads to a change in the position of the spine. Deformities can touch the cervical spine or other parts of the spine and cause osteochondrosis of the thoracic, cervical, and lumbar spine.
- Bad posture. . . Scoliosis, stooping, arched back, kyphosis, and other postural disorders, even if minor, cause serious spinal imbalances. As a result, the load on the intervertebral discs is unevenly distributed, which provokes their deformation and increased wear. The vertebrae begin to converge, which leads to a violation of the nerve processes, cervical osteochondrosis develops quite quickly. Posture disorders caused by a change in the natural position of the ribs have similar consequences.
- Innervation disorder. . . A decrease in the sensitivity of the nerve roots leads to pathological changes in their structure, as a result of which the displacement and deformation of the cervical vertebrae go unnoticed by the patient. Finally, pain due to sensory disorders is absent.
- Diseases of the internal organs. . . The wrong position of the internal organs, their displacement and lowering due to various disorders of function leads to a violation of the general balance in the body. This greatly affects the position of the spine - the cervical and lumbar vertebrae are displaced and deformed, which leads to the corresponding osteochondrosis.
- Violation of the blood supply. . . Since the intervertebral discs have no direct connection to the circulation, they are supplied with nutrients from the surrounding tissue. A violation of the blood supply to the cervical spine leads to the fact that the intervertebral discs do not receive enough fluid for rehydration (restoration of shape through moisture absorption), renewal of cartilage tissue. As a result, their wear and tear is accelerated, the distance between the vertebrae of the cervical spine decreases, which leads to osteochondrosis.
Stages
The attending physician should determine the degree of development of cervical osteochondrosis based on the anamnesis, as well as the examination of the patient. There are only four grades:
- First degree. . . The disease is in the bud, the patient has mild neck pain, which may become more intense as the person begins to turn his head.
- Second degree. . . The patient may complain of very severe pain in the cervical spine, which may be localized in the upper limbs. The clinical picture shows that at this stage of the development of the disease, pinching of the nerve bundles is observed, causing severe pain. Headache, weakness, and general malaise are also noted.
- Third degree. . . The pain becomes almost incessant and also radiates into the shoulder or arm. Some patients are diagnosed with a herniated disc, which causes loss of sensation in the upper limbs. When examined by a doctor, there is a noticeable decrease in the mobility of the cervical spine, as well as pain on palpation.
- Fourth degree. . . At this stage of the disease, the intervertebral disc is almost completely destroyed. In its place, connective tissue appears, which leads to the deterioration of the patient's condition. He begins to feel more pain, noises in the head and poor orientation in space. This suggests that the artery is pinched, which is disrupting the brain's natural nutrition.
First signs
How osteochondrosis of the cervical spine manifests itself:
- radicular syndrome - against the background of compression of the nerve endings, pain appears, spreading from the neck to the shoulder blades, forearms and anterior chest wall;
- Muscle weakness in the arms, noticeable swelling of the neck;
- when moving the head, a characteristic crunch is heard;
- Weakness, chronic fatigue, drop in blood pressure;
- lack of coordination, often dizziness, seizures are accompanied by nausea, vomiting;
- Visual and hearing impairment, noise, ringing in the ears;
- Numbness of limbs, tongue;
- frequent migraines;
- women between the ages of 45 and 65 experience pain, numbness and tingling in the upper extremities during sleep; seizures can be repeated several times a night.
Symptoms of osteochondrosis of the cervical spine
Important symptoms of cervical osteochondrosis are dizziness, headache, increase in blood pressure.
Diagnosing the disease is difficult, pain sometimes does not appear and symptoms are cleared, in addition, the uncontrolled use of strong analgesics masks the signs of the disease. A patient who does not feel pain considers himself healthy, and this continues until irreversible processes develop in the tissues of the neck joints.
Headache with cervical osteochondrosis
The most common causes of headache in the pathology we describe:
- Vascular spasms of the brain;
- Pinched nerve roots;
- Reflex increase in intracranial pressure.
Feels like the pain can be paroxysmal, constant, throbbing, and dull.
Dizziness in cervical osteochondrosis
Dizziness can result from:
- Inflammation in the middle or inner ear;
- Vascular spasms of the brain;
- Disturbances in the transmission of nerve impulses;
- Problems with the vestibular apparatus;
- Cardiovascular diseases.
There are no clear criteria for dizziness in osteochondrosis. However, there are systemic and non-systemic vertigo, they have obvious differences.
It is recommended that you understand the differences between systemic and non-systemic vertigo. This will help to independently determine the causes of an unusual condition:
- Systemic dizziness is a feeling of circular motion of surrounding objects or the body, which is a result of a disruption of the vestibular apparatus, visual analyzers and receptors in the joints, muscles and epidermis (osteochondrosis of various etiologies);
- Non-systemic dizziness is a feeling of lightheadedness, numbness, of insecurity about being in an upright position. In non-systemic vertigo, the sense of circular rotation is absent, and this is an important difference between the signs compared.
A person who experiences such dizziness should first be examined by an experienced doctor by a neurologist or (if an ear, nose and throat disease is suspected) by an ENT doctor.
The reason for an emergency hospitalization not associated with osteochondrosis of the cervical spine is to identify the patient (other than dizziness) with the following signs:
- Paralysis of the muscles of the face and numbness of part of the shoulder girdle;
- severe headache on the background of a deterioration in health;
- Movement coordination disorders;
- Loss or extinction of consciousness.
Blood pressure in cervical osteochondrosis
The association of cervical osteochondrosis with increases in blood pressure has long been known. The cervical vertebrae have important nerve endings and blood vessels.
A peculiarity of high blood pressure in cervical osteochondrosis is a combination with the following symptoms:
- Headache;
- Pain in the limbs and chest;
- Decreased sensitivity in the neck area;
- The occurrence of pressure surges after stress, muscle tension, prolonged uncomfortable posture and similar situations.
These signs should be taken into account with self-differentiating hypertension of different origins.
Sharp jumps in blood pressure and a rapid deterioration in the state of health are the basis for seeking emergency medical help.
Osteochondrosis Syndromes
Osteochondrosis consists of the following syndromes:
- whirl. . . It is also called a vertebra, which indicates that bone and cartilage tissue are involved in the pathological process. This leads to the formation of such symptoms: restriction of motor activity of the neck, pain when turning, radiological changes in the image of the cervical spine. The simultaneous appearance of these signs is vertebral syndrome. A similar set of clinical symptoms is observed in myositis (muscle tissue pathology), and painful movements are an accompaniment to many other pathologies.
- Heart syndrome. . . It is expressed by a burning sensation in the chest area, the appearance of shortness of breath. The person feels his heartbeat fast, becomes tired and irritable. This picture is also typical of cardiological pathology, for example, angina pectoris, coronary syndrome, myocardial infarction. An exact statement about the causes of such symptoms can be made after an EKG of the patient.
- Radicular Syndrome. . . The neck region innervates 8 pairs of nerves, each of which has roots - the point where the nerve emerges from the vertebra. If they are involved in osteochondrosis, the patient feels a decrease in sensitivity, or vice versa - severe pain. There may be numbness in the back of the head, be it painful, decreased sensitivity of the tongue, behind the ear, pain in the supraclavicular region. Sometimes there are swallowing disorders, movements in the girdle of the upper limbs, numbness of the fingers.
diagnosis
If there are clear signs of cervical osteochondrosis on the face, the doctor will prescribe certain methods to make sure the diagnosis is correct:
- X-ray of the cervical spine. This method is advisable in the early stages of the disease, but may be of no use in more advanced forms.
- CT (computed tomography). It allows you to see structural changes in the vertebrae, but using this method it is impossible to determine the size of the break between the vertebrae.
- MRI. It is considered the most effective diagnostic method for determining cervical osteochondrosis. It is possible to determine the size of the rupture between the intervertebral discs, as well as the degree of their development.
- Your doctor may also order a duplex scan to see if your arteries are not working properly.
Complications of the disease
What is the danger of cervical osteochondrosis:
- frequent migraine attacks;
- Cardiac arrhythmias, atherosclerosis;
- Protrusion, intervertebral hernia, bony growths of the vertebrae;
- severe brain diseases;
- Narrowing of the lumen of the vertebral artery, which leads to the development of VSD, cerebral hypertension, obstruction;
- spinal stroke.
First aid at home for exacerbation of osteochondrosis
Painkillers can be used for severe pain. If analgesics do not provide relief, NSAIDs can be used.
"Distracting" agents are often used, for example the pepper plaster, which does not heal, but only warms the inflamed area and distracts it from the pain. With edema in the area of inflammation, the patient can drink an infusion of herbs or a diuretic for 3-4 days. Can osteochondrosis be cured by such methods? These measures are only temporary, in order to treat the causes, you need to consult a doctor.
How to treat osteochondrosis of the cervical spine
At the initial stage of development, osteochondrosis can be cured without drugs, it is enough to revise the diet, revise the daily regimen and regularly do a number of special exercises. With advanced forms of the disease, effective treatment is possible only with the use of various drugs that will help stop degenerative changes in the vertebrae.
The complex of therapeutic measures must include physiotherapy - electrophoresis with drugs, ultrasound, magnetic therapy, laser therapy. These methods help to cope with pain, inflammation, tissue swelling, improve metabolic processes and blood circulation.
Medication
The main methods of treating osteochondrosis of the cervical spine are drug treatment, physical therapy, massage of the cervical zone, therapeutic exercises for cervical osteochondrosis are especially effective. The main groups of drugs used for this disease include:
| Surname | Working principle |
| Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). | They relieve pain, relieve aseptic inflammation and edema of the root of the damaged nerve. |
| Drugs that improve the rheological properties of blood and blood flow. | Improves the nutrition of damaged nerve roots and improves blood flow to the brain. |
| B vitamins. | Improves metabolic processes in nerve tissue. |
| Muscle relaxants. | These are drugs that help relieve muscle spasms. |
| Chondroprotectors. These are glucosamine and chondroitin. | These are drugs that restore cartilage tissue, including in the damaged disc. |
When taking pills for osteochondrosis, it should be remembered that drug treatment with pills will have a significant effect only if you combine them with other methods, including exercise. It should also be noted that the attending physician must prescribe the treatment of the disease based on its stage and other signs.
Many doctors believe that injections are effective as a treatment for cervical osteochondrosis, as it allows for faster action on the nerve endings and minimizes side effects. At the same time, vitamins are best taken in tablet form, since there is no difference in how they are absorbed, but injections can be painful.
Injections for treatment:
- intramuscular injections are generally tonic and anti-inflammatory;
- Blockages are injected directly into the affected area, resulting in a quick effect.
Ointments and gels for external use
This is the most accessible group of drugs for home use. They are divided into anti-inflammatory, warming and pain relievers.
With cervical osteochondrosis, not all ointments are effective, moreover, due to their availability, they are sometimes used inappropriately and without taking into account the peculiarities of the pathogenesis. Before taking any medication, you need to get examined by a doctor.
Exercise therapy
Physiotherapy for cervical osteochondrosis should be carried out without an acute exacerbation. The greatest efficiency of this technique is during the recovery phase. There should be no discomfort and pain during the execution of the complex!
| Exercise number 1 | Lie on your stomach, put your hands on the floor, raise your head and torso, your back should be straight. Remain in this position for 1-2 minutes. Slowly lower yourself to the floor. Repeat 2-3 times. |
| Exercise number 2 | Lying on your stomach, straighten your arms over your body, turn your head to the left, trying to touch the floor with your ear, then turn your head to the right. Repeat 6-7 times in each direction. |
| Exercise number 3 | In a sitting position, bend forward as you inhale and try to touch your chest with your head, then exhale, bend back and tilt your head back. Repeat 10-15 times. |
| Exercise number 4 | While sitting, place your palms on your forehead, applying pressure to your forehead with your palms, and your forehead to the palms of your hands. Continue this exercise for 30 seconds. Repeat 2-3 times. |
| Exercise number 5 | Slowly turn your head one way first, then the other. 10 turns in each direction. Watch out for dizziness. When it appears, the exercise will end. |

Massage for cervical osteochondrosis
The massage must be done carefully and without exerting force. An inexperienced, unprofessional massage can lead to failure. The movements should extend to the cervical spine, collar area, and part of the back. The massage takes place in the prone position, in extreme cases also while sitting.
The techniques are based on the following techniques:
- Stroke. Effects on the surface layers of the skin. With the palms or fingertips from the head to the upper third of the middle of the back. The painting from the base of the neck can also be done in a zigzag pattern;
- To squeeze. Effect on the deep layers of the skin in the upper third of the back. Fingers (thumb and forefinger) above the neck make movements to grip the skin that are reminiscent of squeezing. This is done carefully, tissues near the vertebrae are not affected;
- Trituration. The purpose of the procedure is to warm up the skin and increase blood flow to the neck area. This is done with extreme caution. Effects on the spinous processes of the vertebrae are not allowed. Rubbing can be replaced by sawing movements or circular strokes;
- Knead. It is of limited concern as it affects very deep tissues, which can worsen the pathology.
Self-massage for cervical osteochondrosis is performed in a comfortable sitting position. Stroking methods, circular rubbing in the neck or on the shoulders are used. It is advisable to combine the self-massage method with rubbing in various ointments that stimulate blood circulation and relieve pain in the kneading area.

physical therapy
Along with taking medication, the patient must undergo physiotherapy procedures. They increase the effectiveness of drugs and promote the recovery of joints and intervertebral discs.
- Electrophoresis - The ions of the anesthetic penetrate the painful area due to the action of an electric current.
- Laser therapy - has anti-inflammatory properties, guarantees an improvement in blood circulation through exposure to light.
- Magnetic field therapy - relieves tissue swelling, has an analgesic effect.
- Ultrasound - improving metabolic processes, relieving pain, relieving inflammation of the damaged areas.
Several procedures are used in the form of physiotherapy. The doctor prescribes treatment, relying on the indications and the absence of contraindications.

Home remedies
Alternative treatment must be used as an adjunct to drug therapy and physical education, unconventional methods will not help to get rid of the disease completely.
What to do at home with cervical osteochondrosis:
- Pour boiling water over a fresh horseradish leaf, cool a little, attach the inside to the neck, secure with a thin natural cloth. The procedure is carried out before bedtime, leave the compress on overnight.
- Grate raw potatoes on a fine grater, mix in equal proportions with warm liquid honey. Use the mixture for compresses, the procedure should be carried out 1-2 times a week.
- Mix a raw egg with 100 ml of sunflower oil, 20 ml of vinegar and 20 g of flour, remove the mixture in a dark place for 48 hours, remove the film from the surface. Means to coat the inflamed area before bed, keep in the refrigerator.
- In May, collect pine buds up to 2 cm long, cut into thin slices, fold in a container made of dark glass. For 1 part of the raw material, take 2 parts of sugar and remove the medicine in a dark place for 2 weeks. Drink 5 ml of the mixture three times a day, do not swallow immediately, hold in mouth for 2-3 minutes. Course duration - 15-20 days, repeat 2-3 times a year.
- Grind 150 g of peeled garlic and 400 g of cranberries, put the mixture in a glass container, after 24 hours add 800 ml of honey, mix. Take 5 ml of the drug before meals three times a day.
Cope with severe pain, pull out excess salt with a cabbage leaf smeared with honey, fix the compress on the neck with a warm scarf and leave it on overnight.
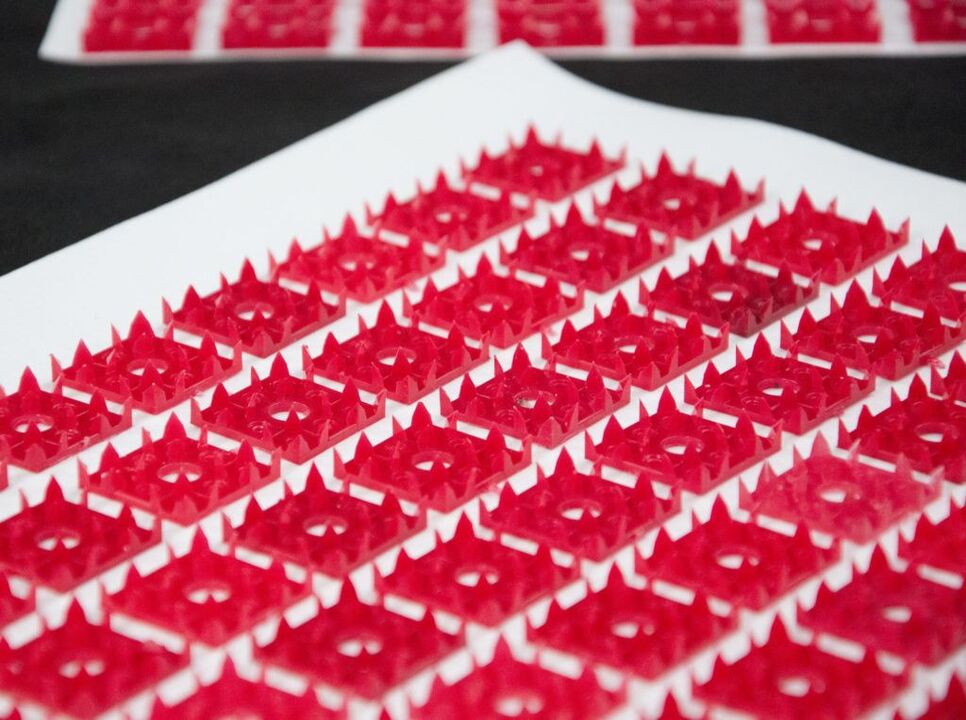
Applicator
The use of applicators is one of the methods of therapy for diseases of the spine, including osteochondrosis.
The effect of the device on the cervical spine normalizes metabolic processes, relieves pain, increases muscle tone, improves blood circulation, increases the conductivity of nerve tissue, etc.
Manual therapy
Manual therapy is based on the principle of restoring motor functions and mobility between the vertebrae.
The manipulations initially consist of a light relaxation massage, then the doctor uses more and more force, acting on the vertebrae by pressing and turning the neck.

surgery
The spine is the foundation of the entire human body. When diagnosing a pathology related to the spine, specialists try to eliminate it therapeutically. Any operation on the spine is life-threatening.
With cervical osteochondrosis, surgical intervention is allowed under the following indications:
- Intervertebral hernia, spondylolisthesis, spinal stenosis;
- missing treatment results after exposure for more than six months;
- the formation of osteophytes.
Modern medicine offers many options for performing operations with minimal risks to the patient's health and life.
prophylaxis
Cervical osteochondrosis is a disease that mainly develops with an improper lifestyle. Accordingly, disease prevention is a healthy lifestyle.
It is possible to reduce the risk of developing SHO if:
- exclude provoking factors;
- do sports regularly;
- do not resort to heavy physical activity;
- getting rid of bad habits;
- try to be as little nervous as possible;
- eat properly.
Adhering to preventive measures will help speed up the healing process and eliminate the likelihood of relapse. Older people and people with a hereditary predisposition are advised to adhere to prevention at all times. Following a diet and performing simple exercises will definitely produce a positive result. Yoga and swimming are also helpful.





















